From Suspect to Action: Chart w/GPT delivers In-Year ROI and Future-Proof Risk Adjustment for MSOs
.png?width=360&height=176&name=image%20(17).png)
See Chart w/GPT in Action
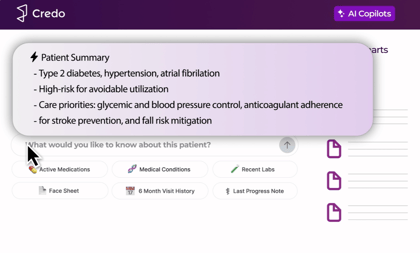
Credo Health built Chart w/GPT to improve patient health and to increase physician engagement with HCC suspects at the point of care.
Last fall, Credo Health launched a beta and 150+ doctors signed up. This post synthesizes what those physicians told Credo Health they like, what they want next, and what the team is building toward.
This update summary shows MSO financial and risk leaders how Credo Health uses AI to improve patient health, lower costs immediately, and future-proof risk adjustment in value-based contracts by deploying clinically trained LLMs at the point of care.
When physicians can see complete clinical records and review source-cited HCC suspects inside the visit, it changes real-world behavior.
What Credo Health is finding is that when clinicians trust the insights in front of them and can act quickly at the point of care, review and acceptance rates rise, documentation becomes more defensible, and in-year performance improves across risk and quality programs.
TL;DR for MSO financial and risk leaders
The workflow Credo Health is designing around drives two outcomes that matter for MSOs:
In-year ROI
- Reduce chart chase and operational waste by delivering decision-ready context during the visit.
- Increase realized RAF capture by improving physician review and acceptance of HCC suspects at the point of care.
Future-proof risk adjustment
- Build more complete, defensible documentation that holds up as models and audits evolve.
- Reduce program leakage by ensuring suspects move from identified to reviewed to accepted to billed and paid.
What physicians are saying, and why it matters to contract performance.
1) Trust is created by evidence, not a score
Physicians consistently said they will not act on a suspect unless they can see the supporting proof quickly.
Why it matters to MSOs: source-cited suspects reduce friction, increase adoption, and improve acceptance rates. This is the bridge between “insights generated” and “value realized.”
“This line is very valuable… I’d want an asterisk that says how we know this is true.” — Primary care physician
2) “Documents or it didn’t happen” is a revenue reality
Quality teams often need the actual report filed to earn credit. Physicians want the ability to find and retrieve evidence without jumping between portals.
Why it matters to MSOs: evidence capture impacts Stars and HEDIS performance, reduces rework, and supports audit defensibility.
“You don’t get credit unless you have the document… Links to direct documents will be incredibly handy.”
— Quality operations leader
3) Risk stratification needs to trigger action immediately
What clinicians want at the top is utilization and stability signals that tell them where to deploy resources now.
Why it matters to MSOs: earlier identification and intervention can reduce avoidable utilization and improve in-year contract economics.
“Give utilization up top so I know to deploy resources now.” — Primary care physician
4) “First-pass resolution” drives adoption and reduces leakage
If the evidence is attached, physicians will act and move on. If it is not, suspects get ignored or deferred.
Why it matters to MSOs: first-pass resolution is how programs reduce leakage and increase point-of-care closure.
“If the evidence is there, I accept it and move on.” — Primary care physician
What landed well in the beta
- Curated prompts outperformed ad-hoc free text because they standardize outputs across providers and clinics.
- Preventive views worked best when they paired status with clear next-due logic and rationale.
- ED and hospitalization summaries that read like a case manager brief were consistently valuable.
- A one-page, source-cited face sheet for new patients was called a game changer.
“Basically, this is wonderful. I spent two minutes and have a great understanding of this person.” — Primary care physician
 What physicians want (and what we’re building next)
What physicians want (and what we’re building next)
- Citations and “open document” links on every critical line - live now
- Stronger guideline fidelity and rules that do not drift - ongoing
- A utilization topline metric at the top of summaries - live now
- Stability cues by condition (diabetes, COPD, HF) - ongoing
- One New-Patient Snapshot that assembles meds, preventive, risk, and actions in one step - ongoing
- EMR-friendly export (1–2 pages) that can be filed and reused - in development
- More consistent performance and less response lag - ongoing
The key takeaway
This is not AI for novelty. It is AI infrastructure that turns fragmented records into decision-ready, source-cited insights and places them inside the clinical workflow so physicians actually act.
When that happens, MSOs see:
- Higher physician engagement with HCC suspects at the point of care
- Higher acceptance rates because evidence is immediately visible
- More defensible documentation for audit readiness
- Better in-year performance and a stronger long-term risk adjustment foundation
 Free pilots available
Free pilots available
If you are a financial or risk leader at an MSO, Credo Health would welcome the chance to run a free pilot and show how Credo Health can deliver:
- In-year ROI through immediate operational savings and higher realized capture
- Future-proof risk adjustment through complete records and LLM-driven, source-cited suspects that increase physician review and acceptance at the point of care
Reply to this note or reach out to Credo Health to set up a pilot and define the success metrics that matter most (cost savings, engagement and acceptance rates, audit defensibility, and realized RAF impact).
For a complete rundown of our platform, please watch this video.
Back to blog

.png?width=420&height=205&name=image%20(17).png)
.png?width=420&height=297&name=Credo-25-Chart-ProductValidation-Inspect%20(1).png)
