AI Can Rescue Healthcare From CMS' "Do More with Less" Era

January delivered a rare thing in American healthcare: a coherent signal.
First, the Centers for Medicare & Medicaid Services proposed keeping Medicare Advantage payments essentially flat for 2027—an average net increase of just 0.09%. (Reuters). That's not a rounding error to the people building budgets. It's a message: stop assuming the next year will make up for the last one.
At the same time, Washington continues to relitigate the most emotionally charged word in health policy: "cuts." Every serious attempt to slow the growth of federal healthcare spending gets framed as a moral catastrophe and an assault on vulnerable people.
But here's the uncomfortable truth: the American healthcare industry—payers, vendors, providers, and lobbyists alike—has grown dependent on borrowed federal dollars, and it has become exceptionally skilled at telling voters that any restraint is cruelty.
The 2025 fight over Medicaid spending in the "One Big Beautiful Bill Act" is our most recent example. The healthcare industry's response was to position it as inflicting massive cuts to Medicaid with an avalanche of messaging designed to make any spending restraint feel like a direct threat to human life.
If you step back and look at the actual spending that sits behind the rhetoric, you get the real story: Federal Medicaid grants climbed from $409B in 2019 to $616B in 2023 — a 50% jump in four years, roughly 12.5% per year. The "One Big Beautiful Bill" increases Medicaid grants from $655.9B in 2025 to $860.5B by 2034. That's 31.2% growth over 10 years, roughly 3% per year.
Neither is a "cut." Both are increases and exceed the Federal Reserve's annual inflation target of 2%. The difference is that a 12.5% annual growth rate allows for a lot more inefficiency in the U.S. healthcare system than a 3% target.
You can argue the policy merits either way. My point is simpler: when a system gets used to large, fast, automatic increases, anything less feels like an existential threat, and that panic becomes a business strategy.
The "Do More with Less" Era is Here
Pair the Medicaid debate with the Medicare Advantage proposal and you can see the outline of the next few years: tighter payment, louder scrutiny, higher expectations.
CMS didn't just float a near-flat update; it also proposed a very specific credibility test: starting in 2027, diagnoses from "unlinked" chart review records—those not tied to a beneficiary encounter—would no longer count for risk scores. (CMS) That's a shot across the bow to the entire risk-adjustment ecosystem: if the documentation isn't clinically grounded and auditable, don't expect to get paid for it.
If you run a health plan, an MSO, an ACO, or a clinic taking downside risk, that's not a technical footnote. That's a forcing function. Accuracy and defensibility aren't "nice-to-haves" anymore; they're table stakes.
Davos Made the Subtext Explicit
Then came Davos and the World Economic Forum orbiting it, where healthcare leaders and policymakers spent January openly discussing the lever nobody wants to pull until they have to: productivity.
At an Axios event in Davos, Dr. Oz argued that AI and robotics can already deliver meaningful care and that the most significant changes will come in the next few years—not a decade from now. (Axios) Whether you agree with his timelines or not, the direction is unmistakable: the political class is increasingly comfortable saying out loud what operators have been whispering for years—our current cost structure and labor model can't hold.
And from a media standpoint, it was telling where this conversation played out. Instead of a carefully massaged segment on a traditional Sunday show, Dr. Oz took his case to the All-In Podcast—a long-form forum where ideas aren't reduced to seven-second clips. (YouTube) The show's hosts position themselves as politically diverse, but one of them, David Sacks, is also a White House AI and crypto adviser in the Trump administration. (Reuters) That's not a side note. That's a distribution strategy: go direct, skip gatekeepers, and speak to the tech and business builders you want pulling the next set of levers.
Healthcare Has Tried "More Money." It Hasn't Tried "Better Tools."
 For 20 years, nearly every big promise in healthcare has been some variation of compassionate financing: expand coverage, subsidize access, create new payment models, and trust that costs will eventually follow. Costs didn't follow. Americans still don't feel healthy. Clinicians are still burning out.
For 20 years, nearly every big promise in healthcare has been some variation of compassionate financing: expand coverage, subsidize access, create new payment models, and trust that costs will eventually follow. Costs didn't follow. Americans still don't feel healthy. Clinicians are still burning out.
Even now, burnout remains widespread—43.2% of physicians reported at least one symptom in 2024 —and time spent on after-hours administrative work ("pajama time") remains a major contributor. (American Medical Association)
Here's the irony: in most industries, when productivity is the problem, better software is part of the solution. In healthcare, clinicians are still trapped in slow, non-intuitive workflows designed for billing and compliance first—and patient care second. Everyone who works with clinicians knows the feeling: smart people forced to behave like data-entry clerks.
We love to blame the individuals. We rarely blame the tools.
I'll resist the obligatory pile-on to Epic Systems. This is bigger than one vendor. It's about a system that tolerated mediocre tech because the business model could tolerate mediocre tech.
In most markets, when money is tight, organizations modernize. They don't do it because they're virtuous; they do it because they have to. January's policy signals suggest that "have to" is arriving.
What We've Learned Building AI for the Messiest Data in Medicine
At Credo Health, we've spent our time in the most unglamorous corner of AI: unstructured medical records—PDFs, faxed notes, scanned hospital documents, fragmented histories that don't line up neatly in a database.
In value-based care, that mess matters because clinicians and coding teams are asked to identify gaps and risks that may be present but undocumented. In this context, "HCC suspects" are potential Hierarchical Condition Category diagnoses that appear supported by the record but still require clinician confirmation.
Here's the lesson we keep relearning: more data is not the answer. Better presentation is (See our white paper).

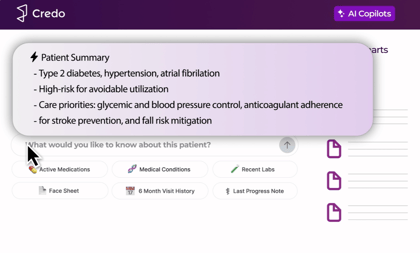
When AI turns chaos into a clear, chronological, sourced narrative— easy to verify—clinicians are far more able and willing to engage. In early work, we've seen triple-digit improvements in physician engagement with these suspected gaps when the information is organized, transparent, and tied back to the original source.
That matters for payment integrity, yes. But it matters even more for care: missed conditions aren't just "missed codes." They're missed chances to catch disease earlier, reduce long-term costs, and sometimes save a life.
The Opportunity Hidden Inside the Pressure
So what does January mean?
It means the era of easy money is fading, which will feel brutal if your strategy depends on the next rate increase to cover last year's inefficiencies.
But it also means we may finally get the modernization in healthcare that has been avoided for decades. When you can't paper over broken workflows with bigger checks, you stop protecting sacred cows. You ask hard questions. You rebuild. You adopt tools that reduce the burden rather than shifting it.
In other industries, this is how transformation happens. A decade ago, when Elon Musk put early Tesla vehicles on the road, many people treated them as a novelty. Today, EV-first automakers are major public companies—Rivian, Lucid Group, NIO, XPeng, VinFast—with market caps that move daily and a combined valuation that still reaches into the tens (and, with Tesla, hundreds) of billions. (StockAnalysis)
Healthcare doesn't need a cult of disruption. It just needs practical innovation that gives clinicians back time, improves documentation quality, and makes care more consistent—not just more expensive.
January's message was a demand for better results, better proof, and tighter budgets.
If we take that signal seriously, we might finally build a healthcare system where technology helps the people doing the hardest work—and where patients get a system that is not only funded but also functional.
Back to blog

.png?width=420&height=205&name=image%20(17).png)
.png?width=420&height=297&name=Credo-25-Chart-ProductValidation-Inspect%20(1).png)