Future-Proofing Risk Adjustment: 3 Essential Changes to Embrace Today

It’s 2024, and we’re living in a digital world. Yet far too many healthcare providers are making do with outdated and incomplete methods for collecting, analyzing, and using medical records.
With the rollout of CMS-HCC V28, the publication of TEFCA 2.0, and the continued push for national interoperability, now is the time for value-based care organizations to augment their risk adjustment efforts with better technology and additional support.
There are 3 key areas that require the most attention as we adapt to the changing landscape: medical records retrieval processes, record structure and readability, and the automation of manual processes.
What’s Changing with HCC Coding?
Under the V28 model, more than 2,000 ICD-10 codes have been removed from the current risk adjustment model. This means that providers have to be much more precise with their diagnoses to avoid missing out on premiums.
Incorrect or unsupported diagnoses can result in payment retraction or fines during Risk Adjustment Data Validation audits.
On the other hand, overlooking a diagnosis lowers the patient's RAF score and adversely affects the provider's premium from CMS.
These consequences were already a significant source of concern for at-risk provider groups. But now that the list of HCC codes is shrinking, it’s more important than ever to code accurately and to catch all diagnoses.
And yet, the current systems for medical retrieval, storage, and analysis are not sophisticated enough to give providers the support they need for accurate, efficient coding under these new rules.
3 Areas Value-Based Care Groups Should Focus On
Unfortunately, our current systems for medical record retrieval, storage, and analysis are not equipped to support accurate coding under these new rules. Here are the three critical areas that value-based care groups should focus on to prepare for the upcoming changes.
1. Medical Records Retrieval Process
In order to succeed at risk adjustment, providers need a complete and accurate understanding of the patient’s entire medical history. Unfortunately, our current systems and processes are not enabling providers to even access that information, let alone analyze it.
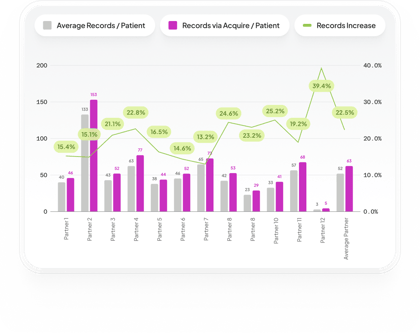
Even with the implementation of EHRs, 78% of hospitals are still “often or sometimes” using mail and fax to receive medical records. This wastes an enormous amount of the clinical staff’s already limited time, and it’s difficult to know for sure if you’ve found all the important records.
If you’re only looking at records within your existing EHR — or the limited records you were able to gather through manual chart chasing — it’s nearly impossible to do comprehensive HCC coding.
2. Record Structure and Readability
Even when organizations are able to retrieve patient medical records, they’re often incomplete, illegible, or contain far too many pages for a provider to read and analyze before the clinical encounter.
The creation of FHIR standards was a step in the right direction, but they only began to solve the problem of record readability and interoperability. Up to 70% of clinical value is documented within unstructured progress or SOAP notes, and there’s no efficient way for coders to extract that information.
To solve this problem, organizations need to look outside of manual processes and consider the potential of artificial intelligence and machine learning.
These systems can process enormous amounts of data in a variety of formats, compiling a list of potential diagnoses and ICD-10 codes for the provider and manual risk adjusters to review.
3. Automation of Manual Processes
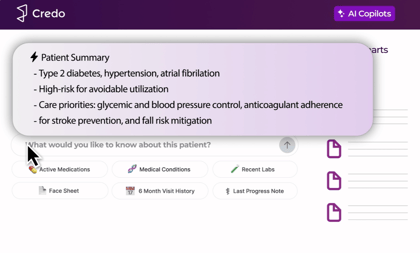
Automation tools will be crucial for successful risk adjustment under HCC V28. By automating records analysis, providers can shift to pre-encounter risk adjustment, creating value for at-risk providers and improving patient outcomes.
There’s also enormous potential for AI to help coders extract value from the unstructured progress or SOAP notes, including diagnoses, prescriptions, and even specific treatment plan details.
By leveraging AI and ML models to augment current risk adjustment efforts, providers could walk into clinical encounters with a list of diagnoses to address and a comprehensive understanding of the patient’s medical histories and current needs.
Tap into the Power of Digitized Records
At Credo, we’re committed to helping MA providers remain compliant while maximizing value for all involved parties.
Our cutting-edge solution offers a first-of-its-kind pre-encounter patient summary that automates the discovery of diagnostic codes and identifies care gaps within medical records. We pair this technology with human coders who can add, remove, or modify ICD-10 codes as needed.
To learn more about how Credo can work for you, simply fill out this form to get in touch.
Back to blog
.png?width=420&height=205&name=image%20(17).png)
.png?width=420&height=297&name=Credo-25-Chart-ProductValidation-Inspect%20(1).png)