00-BackgroundGradient
05-HeroSimpleText
05-HeroSimpleText
Credo Health for Health Plans
Empowering Health Plans to Succeed in Risk Adjustment & Value-Based Care.
Delivering accurate coding, actionable insights, and compliant documentation at scale through clinical intelligence.
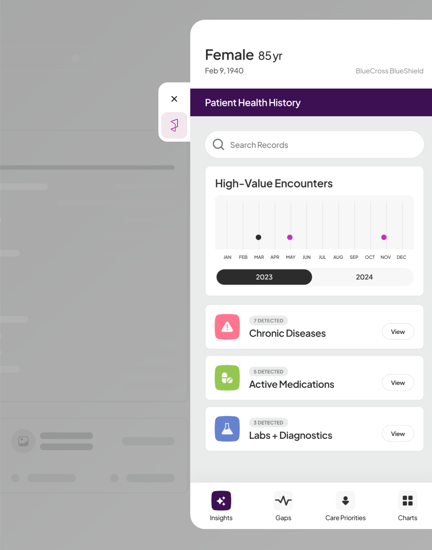
Credo Health helps health plans succeed across Medicare Advantage, Medicaid, and ACA lines of business by solving four critical challenges: missing data, hidden insights, clinical engagement and process optimization.
101-cards-with-nav
103-colored-cards
Fully Integrated. Always in Workflow.
Credo integrates seamlessly with leading EHRs:
22-StackedContentCards
06-ContentMedia